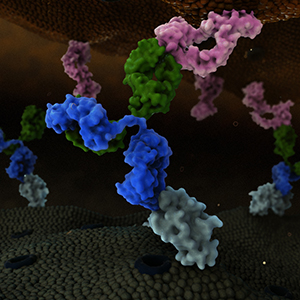
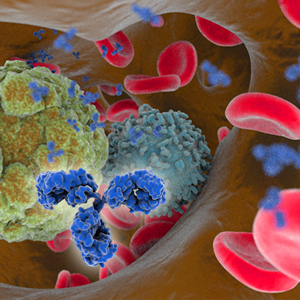
On March 6, 2018, the US Food and Drug Administration (FDA) approved ibalizumab-uiyk (Trogarzo) for adult patients infected with human immunodeficiency virus (HIV) who were previously treated with multiple HIV medications and whose HIV infections are resistant currently available therapies. Ibalizumab-uiyk, a humanized IgG4 monoclonal antibody, is a CD4 domain 2-directed post-attachment HIV-1 inhibitor. The marketing application was granted Breakthrough Therapy, Fast Track and Priority Review designations, and ibalizumab was granted an orphan drug designation by FDA. Theratechnologies Inc. and TaiMed Biologics, Inc. have an agreement to market and distribute Trogarzo in the US and Canada.
The product is administered intravenously (IV) as a single loading dose of 2,000 mg followed by a maintenance dose of 800 mg every 2 weeks after dilution in 250 mL of 0.9% sodium chloride. The safety and efficacy of ibalizumab-uiyk were evaluated in the Phase 3 TMB-301 study (NCT02475629), which was a single arm, multicenter clinical trial conducted in 40 heavily treatment-experienced HIV-infected patients with multidrug resistant HIV-1. At Week 25, viral load <50 was achieved in 43% of patients, while 55% and 48% of patients had a ≥ 1 log10 reduction in viral load and a ≥ 2 log10 reduction in viral load, respectively. The most common adverse reactions reported in at least 5% of subjects were diarrhea, dizziness, nausea, and rash. In total, 292 patients with HIV-1 infection were exposed to ibalizumab-uiyk IV infusion during clinical studies. Additional prescribing information for the drug can be found here.
The Antibody Society maintains a comprehensive table of approved antibody therapeutics and those in regulatory review in the EU or US. As of March 7, 2018, a total of 2 mAbs have been granted first approvals in either the US or EU in 2018, and marketing applications for a total of 9 antibody therapeutics that have not yet been approved in either the EU or US are undergoing review in these regions. Please log in to access the table, located in the Members Only section.
Not a member? Please join! Membership is free for students and employees of the Society’s corporate sponsors.