Antibody Engineering & Therapeutics, held in December 2021, offered many opportunities to hear exciting and informative presentations by experts in the field. We are pleased to present here a summary of a lecture given in the “Immune Cell Recruitment and Redirection” session by Prof. Kerry Chester. The summary was kindly written by Dr. Czeslaw Radziejewski.
Antibody Engineering & Therapeutics, held in December 2021, offered many opportunities to hear exciting and informative presentations by experts in the field. We are pleased to present here a summary of a lecture given in the “Immune Cell Recruitment and Redirection” session by Prof. Kerry Chester. The summary was kindly written by Dr. Czeslaw Radziejewski.
Clinical-stage ROR1xCD3 bispecific antibodies with potential for broad cancer specificity.
Kerry Chester, Professor of Molecular Medicine at University College London and CSO of Novalgen.
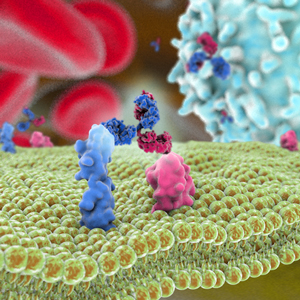
The leading molecule of Novalgen is NVG-111, a first-in-class tandem T-cell engager in single-chain variable fragment (scFv) format. One arm of NVG-111 targets a T-cell coreceptor, CD3, while the second binds to the tumor-associated tyrosine kinase-like receptor ROR1. ROR1 was cloned in 1992 from a neuroblastoma cell line. (1) The function of ROR1 as a tyrosine kinase is still poorly understood, although some studies show evidence of its intrinsic tyrosine kinase activity. ROR1 is a cell-surface oncofetal antigen, expressed during embryogenesis and largely absent in normal adult organs, with only low-level expression on adipocytes, pancreas, and parathyroid glands. In contrast to the lack of expression in healthy tissues, ROR1 is present in a wide range of cancers and cancer initiating stem cells. It is expressed in both hematological malignancies and in solid tumors. (2)
ROR1 has three extracellular domains: Kringle, Frizzled and Ig-like domain. ROR1 sequences of extracellular domain (ECD) are highly similar between different species. For example, there is 97.6% identity between mouse and human ROR1 ECD. Many years after the initial ROR1 discovery, its ligand was identified as Wnt-5a, one of the Wnt family signaling molecules. Unlike other ROR1 clinical candidates under development, the anti-ROR1 arm of NVG-111 binds to ROR1 Frizzled domain.
Novalgen began the development of NVG-111 by immunizing rats with recombinant extracellular domain of ROR1. The majority of the resulting antibodies bound to Ig-like domain, none bound to Kringle domain, and only one clone (clone F) bound to Frizzled domain. Clone F was selected for further development. Using flow-cytometry, Novalgen demonstrated binding of clone F to a large number of human cancer cell lines. Clone F was humanized and used to format a bispecific scFv with humanized anti-CD3. NVG-111 binds to mouse and to human ROR1 with low nanomolar affinity, but the anti-CD3 arm does not bind to mouse CD3.
In preclinical studies NVG-111 was effective in in-vitro and in an in-vivo mice model of hematological malignancies, and it demonstrated the ability to kill solid tumor in an established PANC-1 mouse xenograft model of human pancreatic carcinoma. NVG-111 also demonstrated killing in models of advanced solid tumors. It eliminated CD44+/CD24- cancer stem cells in a solid tumor model of triple-negative breast cancer. It induced dose-dependent killing in chronic lymphocytic leukemia (CLL) patient samples where patient CLL cells were cocultured with autologous T cells with EC50 in the range of 4-100 pg/ml. NVG-111 showed T cell-mediated killing of mantle cell lymphoma (MCL) cells that was as effective as killing by blinatumomab, which binds CD3 and CD19, but with 2—30% lower levels of cytokine release (measured as interferon gamma) than blinatumomab, suggesting lower risk of cytokine-release syndrome. Toxicity studies performed in mice using AAV expressing NVG-111 showed lack of toxicity at levels 20- to 1000-fold of expected steady-state levels in clinical dose. Because over 90% of CLL/MCL patients are ROR1 positive, the current focus of Novalgen clinical studies are these two hematological malignancies. Importantly, ROR1 is not expressed on normal B cells, therefore risk of B cell aplasia is expected to be reduced.
1. Masiakowski P, Carroll RD. A novel family of cell surface receptors with tyrosine kinase-like domain. J Biol Chem. 1992;267(36):26181-90.
2. Yuming Zhao et al. Tyrosine kinase ROR1 as a target for anti-cancer therapies. Front. Oncol., 11:680834. doi: 10.3389/fonc.2021.680834.